Pulmones - Suomen Keuhkosyöpäyhdistys ry
Pulmones - Finlands Lungcancerförening rf
Lung cancer
What is lung cancer?
Lung cancer is a malignant tumor that originates in lung tissue, most often in the cells lining the bronchi. In Finland, it is the third most common cancer among both women and men, with nearly 3,000 new cases diagnosed each year. Although it ranks third in incidence, lung cancer causes more cancer-related deaths than any other cancer.
Most patients diagnosed with lung cancer in Finland (approximately 70%) are between 60 and 79 years of age. Fewer than 10% are under the age of 60 at the time of diagnosis.
🔍 Types
of lung cancer
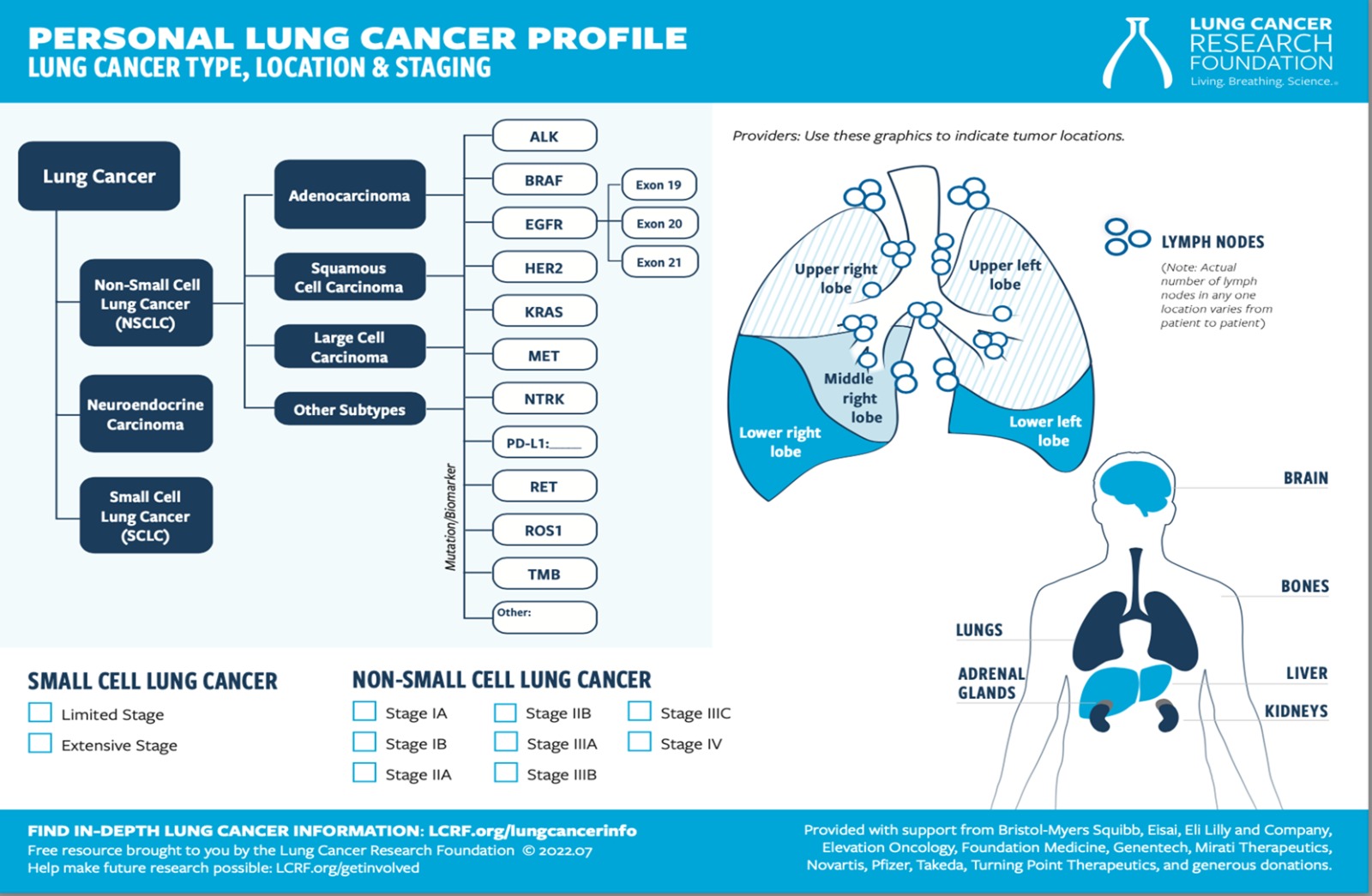
Lung cancer is divided into two main types: non-small cell and small cell tumors which differ in their growth patterns and treatments.
1. Non-small-cell lung cancer (NSCLC)
Non-small cell lung cancer accounts for approximately 85% of all lung cancer cases. The most common subtypes are:
- Adenocarcinoma
- Squamous cell carcinoma
- Large cell carcinoma
In Finland, adenocarcinoma is the most common subtype, accounting for over 50% of cases. It is particularly prevalent among younger patients and never-smokers, and its incidence has been increasing steadily. Squamous cell carcinoma is the second most common subtype (approximately 25%) and occurs more frequently in older individuals and long-term smokers. Large cell carcinoma is the least common subtype and lacks the defining features of the other two. Rare subtypes also exist.
When feasible, the primary aim in non-small cell lung cancer is surgical removal of the tumor.
2. Small-cell lung cancer (SCLC)
Small cell lung cancer accounts for about 15% of lung cancer cases in Finland. It occurs in all age groups, but it is less common in older patients over 80. It is strongly associated with smoking and is characterized by rapid growth and early spread. For this reason, treatment usually relies on systemic therapies rather than surgery.
⚠️ Risk factors
Across the population, several risk factors for lung cancer have been identified. The most significant is smoking. The risk increases with the amount and duration of smoking. The term "pack-year" is used to describe cumulative exposure to tobacco smoke. For example, if someone has smoked ten cigarettes a day for 30 years, that person accumulates 15 pack-years. One can reduce the risk of developing lung cancer by quitting smoking.
Passive smoking (exposure to any kind of smoke) also increases the risk of lung cancer. Occupational exposure to asbestos, radon, arsenic, chromium, nickel, and radon in soil and indoor air, recognized as a risk factor. Long-term exposure to air pollution, especially fine particulate matter (PM2.5), is a well-established risk factor for lung cancer and is considered especially relevant among never-smokers, particularly in urban areas.
A small proportion of patients have a genetic predisposition to lung cancer, although remains under active research. It is important to remember that the exact cause of lung cancer in an individual patient cannot be known for certain.
🔬 Symptoms
Lung cancer may remain asymptomatic for a long
time because the lungs lack sensory nerves. Symptoms often appear only after
the cancer has metastasized (spread) to another organ, or when other symptoms are
present due to the advanced stage of the disease. Symptoms warranting further
examination include persistent cough, coughing up blood, shortness of breath,
chest pain, shoulder or back pain, hoarseness, unexplained weight loss, loss of
appetite, and recurrent lung infections.
🧪 Diagnosis
Many lung cancers can be diagnosed with a standard chest X-ray performed in primary care. Further evaluation typically involves referral to a pulmonary specialist. Diagnostic procedures include computed tomography (CT) scanning and bronchoscopy with tissue sampling. If the tumor is located far from the bronchi, a CT-guided biopsy or endobronchial ultrasound (EBUS) may be used. EBUS enables the detection and sampling of tumors located deep within lung tissue.
Obtaining an adequate biopsy is essential for optimal treatment planning, and multiple attempts might be made. Once a sufficiently representative tumor sample has been obtained, molecular profiling can be performed to identify mutations suitable for targeted therapies. If surgery is considered, staging is usually confirmed with positron emission tomography (PET). Lung function tests, blood tests, and electrocardiography (ECG) are performed to assess surgical and treatment suitability. While no single blood test can detect all lung cancers, circulating tumor DNA may sometimes indicate disease recurrence.
⚙️ Classification of lung cancer
Lung cancer is staged using the international TNM classification. T (tumor) describes the size of the tumor and its possible growth into surrounding tissues, N (node) indicates the spread to lymph nodes, and M (metastasis) refers to metastases (spreading). Based on the TNM classification, lung cancer is generally divided into four stages:
Stage I: Small tumors are present but have not spread to the lymph nodes.
Stage II: Tumors are present and have spread to nearby lymph nodes.
Stage III: Tumors are large or have spread widely to the lymph nodes, but the cancer has not metastasized.
Stage IV: The cancer has metastasized to the other lung, pleura, or other organs.
Small cell lung cancer is typically classified as either limited disease (LD) or extensive disease (ED).
💊 Treatment
The choice of treatment depends on the extent of the disease, the type of lung cancer cells (non-small cell or small cell), and molecular findings including any identified mutations in the cancer cells. The options for treatment are also influenced by the patient's overall health, coexisting conditions, and preferences regarding treatment.
🔪 Surgery
For localized non-small cell lung cancer, surgery is the primary treatment, usually involving removal of one or, less commonly, two lung lobes; in rare cases, it may involve removal of an entire lung. Lung function and overall health must be sufficient to support recovery from the procedure. Surgery can be performed using thoracoscopic or open techniques. Recovery from thoracoscopic surgery is faster than from open surgery.
After surgery, adjuvant treatments, most commonly chemotherapy or targeted therapy may be administered to reduce recurrence risk. These treatments are administered especially if the tumor is large or has spread to the lymph nodes. Sometimes, for larger tumors, medications can be given prior to surgery to shrink the tumor, thereby increasing the likelihood of a successful surgery. This treatment is known as neoadjuvant therapy.
☢️ Radiation therapy
When complete surgical removal of the cancerous cells is not possible, or in situations where surgical treatment is not feasible for other reasons, locally advanced lung cancers can be treated with radiation therapy. In some cases, chemotherapy can be combined with radiation therapy to enhance its effects. Radiation therapy can be administered either as a longer treatment lasting 4-6 weeks (moderate daily radiation doses), or, as in the case of small tumors, as a short, few-session stereotactic radiation therapy (high daily radiation doses). The side effects of radiation therapy typically include reactions in the treated area, usually occurring in the latter half of the treatment or soon after it ends. When lung tissue is irradiated, common side effect is swallowing due to esophageal irritation and mucus buildup.
With high radiation doses, the risk of pneumonia is increased, and it can appear several months after completing therapy. Due to the risk of scarring, planning for radiation therapy aims at minimizing the amount of healthy lung tissue in the radiated area. Radiation therapy can also be used palliatively to relieve symptoms. In this case, radiation course is short, and the total doses are moderate resulting in fewer side effects. The goal is often to alleviate a symptom, such as pain related to a tumor or its metastasis, or bleeding.
💉 Chemotherapy
Chemotherapy (or cytostatics) involves medications that destroy cancer cells or inhibit their growth. It is used as a single agent or in combination with other cancer drugs. The choice of chemotherapy regimen is influenced by factors such as the type of cancer cells, the patient's overall health, and any concurrent
Chemotherapy can be used in advanced disease regardless of the subtype diagnosed. It is also administered before or after surgery in selected cases as adjuvant treatment to reduce the risk of recurrence in patients with non-small cell lung cancer. Chemotherapy is the primary treatment for small cell lung cancer. If small cell lung cancer is limited in growth, chemotherapy can be combined with radiation therapy.
In elderly, frail, or immunocompromised patients, chemotherapy is generally not administered due to the adverse effects, which can include changes in blood cell counts, nausea, fatigue, an increased susceptibility to infection due to weakened immunity, hair loss, peripheral nerve damage (so-called peripheral neuropathy), and decreased kidney function. The incidence of side effects varies across different medications.
Cancers respond differently to chemotherapy. Some cancers respond well to treatment, leading to a reduction in tumor mass, while in other cases, the treatment only prevents the cancer from growing but does not shrink the tumor(s). Some cancers do not respond to chemotherapy, resulting in disease progression during treatment. In such cases, chemotherapy is not beneficial.
🛡️ Immunotherapy
Immunotherapy is also called immunological (or immuno-oncological) treatment. It means using medications that activate the immune system's "killer" cells to recognize and attack cancer cells. These medications are used as single agents, in combination with two immunological drugs, or in combination with chemotherapy agents. Some patients benefit greatly from these drugs, achieving a long-lasting response and tolerating the treatment well. Other patients may not respond or may develop immune-related side effects. The side effects are different from those of chemotherapy and can appear either soon after starting treatment, later during treatment, or even after the medication has been stopped. The side effects result from excessive immune activation, leading immune cells to attack the body's own tissues and causing a condition similar to autoimmune disease.
Immunotherapy can lead to hormonal imbalances or inflammatory conditions in internal organs. The risk of adverse effects is increased when immunological drugs are used in combination.
Tumors expressing high levels of PD-L1, a transmembrane protein that acts as an immune checkpoint, are more likely to respond.
🎯 Targeted therapy
In non-small cell lung cancers, and especially in some adenocarcinomas, mutations can occasionally be found in cancer cells that can be treated with targeted therapies developed for that type of mutation. Many mutations are more common in younger and non-smoking patients. The most common are EGFR and ALK mutations. Less common ones include RET, ROS-1, cMETex14, and NTRK. The presence of mutations is investigated in biopsy samples in the pathology unit; many hospitals in Finland use extensive gene panel tests for this purpose. Generally, the drugs targeted at mutations used to treat advanced lung cancer, but EGFR and ALK mutation drugs can also be used as adjuvant therapy after surgery when the risk of recurrence is increased. At best, targeted therapies can be more effective and less harmful than traditional chemotherapy and are easier to administer because they are tablet-based.
On the other hand, targeted drugs can also have side effects, some of which are serious, and not all patients will benefit from the drugs despite the identified mutation. With advances in cancer medications, new targeted treatments are expected to be introduced in the coming years.
❤️🩹 Palliative care
Palliative care refers to comprehensive treatment provided to patients suffering from incurable lung cancer and to their loved ones. Its aim is to alleviate physical symptoms, strengthen mental resilience, and maintain a good quality of life. Palliative care is often incorrectly perceived as merely end-of-life care, but the palliative phase can be prolonged and quality of life during this time can be good. Visits to a palliative unit can be initiated while the cancer treatment is still ongoing. In this case, the palliative unit focuses on alleviating cancer symptoms, providing mental health support, and guiding patients to social services and practical assistance. Such visits are referred to as palliative concurrent visits or early palliative care.
The palliative care team serves as the responsible unit for the patient's care when curative cancer treatments can no longer be administered. Many attend their first palliative care visit with the belief that nothing more can be done for them. Even though cancer medication has been stopped, there are still treatment options available, and the patient is not left alone with their illness. Depending on the situation and condition, various symptom-relieving medications may be offered, along with advice on improving nutritional status, support for at-home management, care security (for example, access to home hospital services and/or a support place in a ward), and support for mental well-being. Sometimes, a patient who has transitioned to palliative care may also be offered symptom-relieving palliative radiotherapy.
Typically, palliative radiation therapy refers to short-term radiation treatment given for bone metastases to manage pain. Sometimes, palliative radiation therapy can also be given as a short treatment directly to the lung tumor when the tumor compresses the bronchus or large blood vessels or causes hemoptysis (coughing up blood). It is often possible that when heavy and detrimental cancer drug treatments are completed, the patient feels their condition improving and their strength returning.
End-of-life care is the final phase of palliative care, focused on comfort, dignity, and support for patients and their loved ones. When death is approaching, efforts are made to refrain from exhausting treatments and procedures, and to focus on symptom relief, so that death can be peaceful and the presence of loved ones by the patient's side is facilitated. Pain, shortness of breath, and emotional distress can often be effectively managed with medication. By the palliative phase, it is important that a proactive care plan has been created for the patient to anticipate potential new symptoms, allowing them to be treated effectively before they become more troublesome. Home hospitals allow many patients to die at home if they wish. Alternatively, it is possible to transfer to a palliative care home or a palliative support unit before death.
📉 Prognosis
The prognosis of lung cancer largely depends on the stage at diagnosis. Early detection significantly improves outcomes, highlighting the importance of timely evaluation when symptoms occur.
📚 🔗 More information, useful links
Lataa tietoa keuhkosyövästä Terveyskylän keuhkosyöpäosiosta.
Tietoa keuhkosyövästä Syöpäjärjestöjen sivuilta.
Keuhkosyöpäpotilaan opas (Suomen Syöpäpotilaat ry)
Tietoa palliatiivisesta hoidosta Terveyskylän palliatiivisesta talosta.